My treatment approach
Root canal treatment, or endodontic therapy, becomes necessary when the innermost part of the tooth, referred to as the pulp, undergoes irreversible damage usually as a consequence of tooth decay (cavities), trauma, or damage during prior dental procedures (i.e. fillings or crowns). Rather than opting for tooth extraction, root canal treatment often is the preferable choice. Should you need expert endodontic guidance or counsel, your GDP (General Dental Practitioner) may choose to initiate a referral process, particularly if the treatment is complex. Alternatively, you may directly contact me for arranging a consultation. Importantly, your registration with your GDP will not be affected if you choose to have treatment with me. A comprehensive report of all findings and treatments provided will be sent to both you and your dentist. My main priority is that patients:
1.
Feel completely at ease with the entirety of my services.
2.
Understand the problem and alternative solutions.
3.
Understand the various stages of the proposed treatment.
4.
Are aware of costs/timeframes during the consultation process
5.
Are encouraged to engage with me adressing any queries/concerns.
1. What is a root canal treatment?
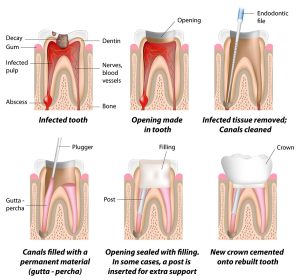
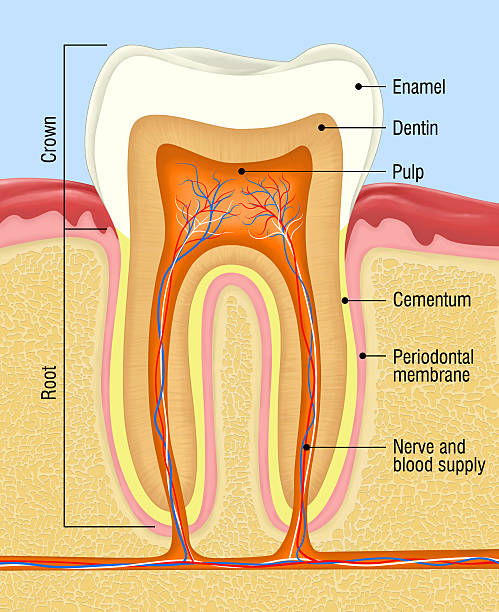
A root canal treatment, also known as endodontic therapy, is a dental procedure aimed at saving a tooth that has become infected or severely damaged by removing the infected pulp and cleaning, shaping, and sealing the tooth’s root canals.
2. Why would I need a root canal treatment?
Root canal treatment is necessary when the pulp inside your tooth becomes infected or inflamed due to deep decay, repeated dental procedures, cracks, chips, or trauma. It is a way to save the tooth and alleviate pain and discomfort.
3. How can I tell if I need a root canal?
Common symptoms that may indicate the need for a root canal include severe toothache, sensitivity to hot and cold, swelling of the gums, a pimple-like bump on the gums, and darkening or discoloration of the tooth.
4. Is a root canal painful?
Contrary to popular belief, modern root canal procedures are relatively painless. Anesthetics are used to numb the area, and advancements in techniques and technology have significantly reduced discomfort during and after the procedure.
5. What happens during a root canal procedure?
During a root canal, your endodontist will remove the infected pulp, clean and shape the root canals, and then seal them to prevent further infection. In some cases, a crown may be recommended to restore the tooth’s strength and appearance.
6. How long does a root canal procedure take?
The duration of a root canal procedure can vary depending on the complexity of the case. Generally, a single root canal treatment can take about 1 to 2 hours, and multiple appointments might be necessary for more complex cases.
7. Are there alternatives to a root canal?
The main alternative to a root canal is tooth extraction. However, saving your natural tooth through a root canal is usually the preferred option as it maintains your bite, jawbone structure, and overall oral health.
8. What is the success rate of root canal treatment?
Root canal treatment has a high success rate, often exceeding 90%. Success depends on factors like proper cleaning and sealing of the canals, the condition of the tooth, and how well it is restored afterward.
9. How should I care for my tooth after a root canal?
After a root canal, you should follow your endodontist’s post-operative instructions, which may include taking prescribed medications, avoiding hard or chewy foods, and maintaining good oral hygiene practices. A follow-up appointment will be scheduled to ensure proper healing.
10. Will I need a crown after a root canal?
In many cases, a tooth that has undergone a root canal will require a crown to protect and strengthen it. The crown restores the tooth’s function and appearance, preventing further damage.
11. Is root canal treatment safe?
Yes, root canal treatment is a safe and routine dental procedure. Modern techniques and sterilization protocols ensure patient safety and successful outcomes.
12. How can I prevent the need for a root canal?
Maintaining good oral hygiene by brushing, flossing, and visiting your dentist regularly can help prevent tooth decay and the need for root canal treatment. Additionally, wearing mouthguards during sports and avoiding biting on hard objects can reduce the risk of dental trauma.
1. What is endodontic microsurgery?
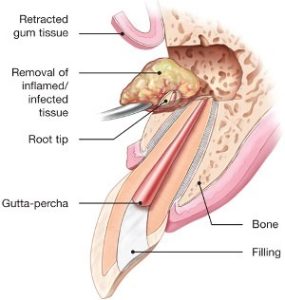
Endodontic microsurgery, also known as apical microsurgery or apicoectomy, is a specialized dental procedure performed under high-powered microscopes. It involves accessing the tip of a tooth’s root to remove infected or inflamed tissue, along with any surrounding damaged bone.
2. When is endodontic microsurgery necessary?
Endodontic microsurgery is typically considered when conventional root canal treatment has not effectively resolved an infection or when a recurrent infection occurs after root canal therapy. It is also used to treat certain cases of root resorption or hidden canals that cannot be treated through traditional methods.
3. How is endodontic microsurgery performed?
During endodontic microsurgery, a small incision is made near the tip of the tooth’s root to access the infected area. Using advanced microsurgical instruments and a high-powered microscope, the endodontist removes the infected tissue, cleans the area, and seals the end of the root with a biocompatible material.
4. Is endodontic microsurgery painful?
Like root canal treatment, endodontic microsurgery is performed under local anesthesia, ensuring that you are comfortable throughout the procedure. Patients may experience mild discomfort after the surgery, which can usually be managed with over-the-counter pain relievers.
5. What are the advantages of endodontic microsurgery?
Endodontic microsurgery offers several advantages, including enhanced visualization of the surgical site, precise removal of infected tissue, and improved success rates in treating challenging cases. It also may be the only option of conserving a tooth where conventional root canal treatment is not feasible.
6. How long does endodontic microsurgery take?
The duration of endodontic microsurgery can vary depending on the complexity of the case. Generally, the procedure can take anywhere from 1 to 2 hours.
7. What is the success rate of endodontic microsurgery?
Endodontic microsurgery has a high success rate, often exceeding 90%. Success depends on factors such as proper case selection, precise surgical technique, and post-operative care.
8. Is endodontic microsurgery the same as a root canal treatment?
Endodontic microsurgery is a different procedure from root canal treatment. Root canal treatment focuses on cleaning and shaping the internal canals of the tooth, while endodontic microsurgery involves accessing the root tip and surrounding areas through a small incision.
9. How long is the recovery period after endodontic microsurgery?
Most patients can resume normal activities within a day or two after endodontic microsurgery. It is advisable to avoid strenuous activities and follow your endodontist’s post-operative instructions for optimal healing.
10. Are there any alternatives to endodontic microsurgery?
In cases where endodontic microsurgery is not feasible or successful, the alternative may be tooth extraction. Your endodontist will recommend the most suitable treatment option based on your specific condition.
11. Can any endodontist perform microsurgery?
Endodontic microsurgery requires specialized training and equipment. It is typically performed by endodontists who have received advanced training in microsurgical techniques and have access to high-powered microscopes.
12. How can I prepare for endodontic microsurgery?
Your endodontist will provide you with specific instructions to prepare for the procedure, including guidelines for fasting, medications, and transportation to and from the clinic.
1. Why is an initial consultation important?
The initial consultation is a crucial step in your endodontic journey. It allows me to assess your dental health, discuss your concerns, and develop a personalized treatment plan tailored to your needs.
2. What can I expect during the initial consultation?
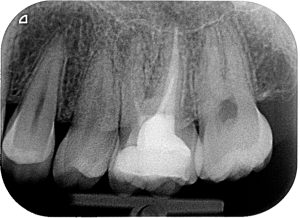
During the initial consultation, I will conduct a comprehensive examination of your oral health, which may include X-rays, visual assessments, and discussing your medical history. This helps me accurately diagnose your condition and recommend appropriate treatment options.
3. How is the diagnosis made?
I utilize advanced diagnostic tools and techniques, including digital imaging and clinical assessments, to accurately diagnose your dental issue. I will thoroughly explain my findings and ensure you have a clear understanding of your condition.
4. Will I be informed about my treatment options?
Absolutely. I believe in patient-centered care, and discussing treatment options is a vital part of my process. I will explain all available options, their benefits, potential risks, and associated costs to help you make an informed decision about your care.
5. What is informed consent, and why is it important?
Informed consent is your right to have a comprehensive understanding of your proposed treatment, including its purpose, potential outcomes, risks, and alternatives. It empowers you to make an educated decision about your dental care and ensures you are an active participant in your treatment plan.
6. What happens if I don’t understand the treatment options or information provided?
I am dedicated to ensuring you have a clear understanding of your condition and the available treatment options. I encourage you to ask questions, and I will take the time to provide detailed explanations until you feel confident in your decision.
7. How do I prepare for the initial consultation?
To make the most of your consultation, it’s helpful to bring any relevant dental records and X-rays (if you are not being referred by a general dental practitioner), and a list of medications you are currently taking. Additionally, prepare any questions or concerns you may have about your dental problem.
8. How long will the initial consultation take?
The duration of the initial consultation can vary based on your individual needs and the complexity of your case. On average, it may take about 30 minutes to complete the assessment and discussion.
9. Can I bring a family member or friend to the consultation?
Absolutely, you are welcome to bring a family member or friend for support and to help you remember the information discussed during the consultation.
10. Will I receive a treatment plan after the consultation?
Yes, following the consultation, I will provide you with a personalized treatment plan that outlines the recommended procedures and associated costs.
11. Is the initial consultation covered by insurance?
Many dental insurance plans cover the cost of an initial consultation, but coverage can vary. You may need to discuss what is included with your insurance provider.
12. How do I schedule an initial consultation?
Scheduling an initial consultation is easy. Your general dental practitioner will be able to advise you and refer you to me. Alternatively, you can contact me directly on one of my practices to request an appointment. Our friendly staff will work with you to find a convenient time for your consultation.
After Root Canal Treatment:
1. What should I expect immediately after a root canal treatment?
After a root canal, you may experience some mild discomfort or sensitivity. This is normal and can usually be managed with over-the-counter pain relievers. In some cases, the discomfort/pain may last up to 5 days and peak around day 3 or day 4.
2. How can I care for my tooth after a root canal?
It’s important to practice good oral hygiene. Avoid chewing on hard or sticky foods, and follow any specific instructions provided by your endodontist. Attend your follow-up appointments for proper monitoring.
3. Can I eat and drink normally after a root canal?
You may need to avoid eating on the treated tooth temporarily, especially if a final restoration like a crown is not yet in place. Follow your endodontist’s recommendations for dietary restrictions.
4. What if I experience a flare-up of pain after root canal treatment?
In rare cases, a flare-up of pain or swelling may occur after root canal treatment. Contact your endodontist if you experience persistent or severe discomfort, as further evaluation may be necessary.
After Endodontic Microsurgery:
1. What can I expect in the immediate aftermath of endodontic microsurgery?
Following endodontic microsurgery, some swelling and discomfort are common. Applying ice to the area and taking prescribed medications can help manage these symptoms.
2. How should I take care of the surgical site after endodontic microsurgery?
Keep the surgical area clean and follow any post-operative instructions provided by your endodontist. Avoid strenuous activities and adhere to a soft-food diet if recommended.
3. Is it safe to smoke after endodontic microsurgery?
It’s highly advisable to avoid smoking after endodontic microsurgery, as smoking can hinder the healing process and increase the risk of complications. Smoking may delay recovery and affect the outcome of the procedure.
4. When can I resume physical exercise after endodontic microsurgery?
Engaging in strenuous physical activities immediately after endodontic microsurgery may impact the healing process. It’s best to follow your endodontist’s guidance on when it’s safe to resume exercise. Light activities and walking are usually recommended during the initial recovery period.
5. Can I resume my regular oral hygiene routine after endodontic microsurgery?
While it’s important to keep the surgical site clean, be gentle around the area when brushing and flossing. Your endodontist will provide specific instructions on how to care for your oral hygiene during the healing process.
 1. Why is a 1-year review important after endodontic treatment?
1. Why is a 1-year review important after endodontic treatment?
A 1-year review allows us to assess the long-term success of the treatment and ensure that the tooth has healed and it has been restored properly. It’s an opportunity to address any concerns and monitor your oral health progress.
2. What happens during the 1-year review?
During the review, I will perform a thorough examination of the treated tooth and surrounding tissues. I may take X-rays to check for any changes or developments since the initial treatment. Your feedback and any symptoms you’ve experienced will also be discussed.
3. What if I experience discomfort before the 1-year review?
If you experience any discomfort, pain, or unusual symptoms before your scheduled 1-year review, don’t hesitate to contact me. I am here to address any concerns you may have.